Enfermeros en la prevención del cáncer: cómo llegar a los que no se llega
DOI:
https://doi.org/10.54502/msuceva.v2n1a8Palabras clave:
Cáncer, Hábitos de vida, Prevención primaria, Profesionales de la salud, Servicios sanitariosResumen
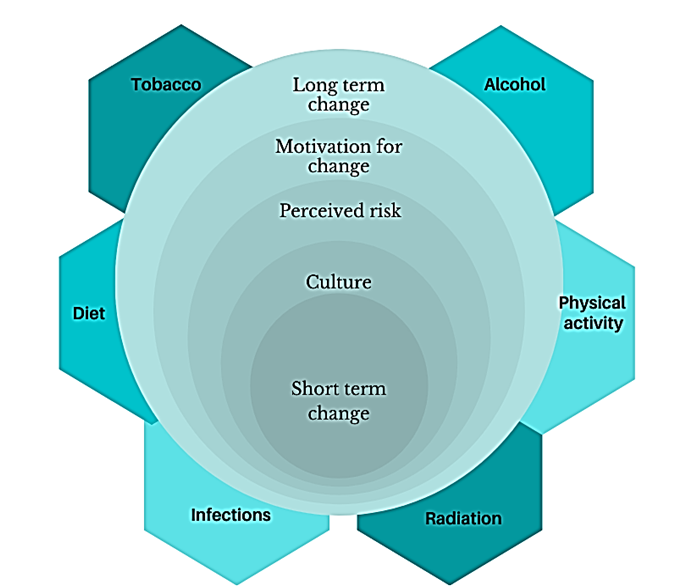
El objetivo de esta reflexión es delimitar estrategias de prevención y formación a profesionales sanitarios sobre el cáncer y sus factores de riesgo, pretendiendo que se involucren más en la promoción de la salud y en la prevención del cáncer, para ayudar a la población a comprender los riesgos individuales e implementar hábitos de vida saludables mantenidos en el tiempo. La prevención presenta una oportunidad para disminuir la carga global que supone el cáncer. En concreto, la prevención primaria, más accesible y menos costosa que la detección precoz del cáncer, podría ayudar a disminuir hasta un 40% de los casos de cáncer que se consideran relacionados a causas modificables como hábitos de vida. Los enfermeros poseen un rol fundamental en la prevención primaria, pero para ello, estos profesionales de la salud, deben tener conocimientos sobre los factores de riesgo del cáncer, comprender cómo se cambian los hábitos de vida y aceptar el papel que tienen en la educación para la prevención.
Descargas
Métricas
Citas
International Agency for Research on Cancer. GLOBOCAN: Estimated number of new cases in 2020, worldwide, both sexes, all ages. WHO. 2020. https://gco.iarc.fr/today/online-analysis-table?v=2020&mode=cancer&mode_population=continents&population=900&populations=900&key=asr&sex=0&cancer=39&type=0&statistic=5&prevalence=0&population_group=0&ages_group%5B%5D=0&ages_group%5B%5D=17&group_cancer=1&i.
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN Estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49. https://doi.org/10.3322/caac.21660 DOI: https://doi.org/10.3322/caac.21660
McCormack V, McKenzie F, Foerster M, Zietsman A, Galukande M, Adisa C, et al. Breast cancer survival and survival gap apportionment in sub-Saharan Africa (ABC-DO): a prospective cohort study. Lancet Glob Heal. 2020 ;8(9):e1203–12. DOI: https://doi.org/10.1016/S2214-109X(20)30261-8
https://doi.org/10.1016/S2214-109X(20)30261-8
World Health Organization. WHO report on cancer: setting priorities, investing wisely and providing care for all. Geneva PP - Geneva: World Health Organization (WHO). https://apps.who.int/iris/handle/10665/330745
Whiteman DC, Wilson LF. The fractions of cancer attributable to modifiable factors: A global review. Cancer Epidemiol. 2016;44:203–21.
http://dx.doi.org/10.1016/j.canep.2016.06.013 DOI: https://doi.org/10.1016/j.canep.2016.06.013
Schüz J, Espina C, Villain P, Herrero R, Leon ME, Minozzi S, et al. European Code against Cancer 4th Edition: 12 ways to reduce your cancer risk. Cancer Epidemiol. 2015 1;39:S1–10. https://doi.org/10.1016/j.canep.2015.05.009 DOI: https://doi.org/10.1016/j.canep.2015.05.009
World Cancer Research Fund International. Our cancer prevention recommendations. WCRF. 2016. https://www.wcrf.org/diet-and-cancer/cancer-prevention-recommendations/
Soerjomataram I, Bray F. Planning for tomorrow: global cancer incidence and the role of prevention 2020–2070. Nat Rev Clin Oncol 2021 1810. 2021;18(10):663–72. https://doi.org/10.1038/s41571-021-00514-z DOI: https://doi.org/10.1038/s41571-021-00514-z
Institute of Medicine (US), National Research Council (US), National Cancer Policy Board, Curry SJ, Byers T, Hewitt M, eds. Fulfilling the potential of cancer prevention and early detection. Cancer Prev Early Detect. 2003;
https://doi.org/10.17226/10263 DOI: https://doi.org/10.17226/10263
Kamaraju S, Drope J, Sankaranarayanan R, Shastri S. Cancer prevention in low-resource countries: an overview of the opportunity. Am Soc Clin Oncol Educ book Am Soc Clin Oncol Annu Meet 2020;40(40):1. https://doi.org/10.1200/EDBK_280625 DOI: https://doi.org/10.1200/EDBK_280625
Diez de los Rios de la Serna C, Fernandez-Ortega P, Lluch-Canut T. CN13 Review of healthcare interventions to promote cancer prevention by improving lifestyle behaviours. Ann Oncol 2021;32:S1260. https://doi.org/10.1016/j.annonc.2021.08.638 DOI: https://doi.org/10.1016/j.annonc.2021.08.638
White LN, Faulkenberry JE. Screening by nurse clinicians in cancer prevention and detection. Curr Probl Cancer1985;9(4):1–42. DOI: https://doi.org/10.1016/S0147-0272(85)80028-3
https://doi.org/10.1016/s0147-0272(85)80028-3
Ayres CG. Said another way. Nurses’ role in cancer control. Nurs Forum. 2009, 44(1):64–7. https://doi.org/10.1111/j.1744-6198.2009.00128.x DOI: https://doi.org/10.1111/j.1744-6198.2009.00128.x
Entrekin NM, McMillan SC. Nurses’ knowledge, beliefs, and practices related to cancer prevention and detection. Cancer Nurs 1993;16(6):431–9.
Sinclair J, McCann M, Sheldon E, Gordon I, Brierley-Jones L, Copson E. The acceptability of addressing alcohol consumption as a modifiable risk factor for breast cancer: A mixed method study within breast screening services and symptomatic breast clinics. BMJ Open 2019;9(6):1–12. https://doi.org/10.1136/bmjopen-2018-027371 DOI: https://doi.org/10.1136/bmjopen-2018-027371
Fernández-Ortega P, Diez De Los Rios de la Serna C. Cancer nurses, are we really contributing to reduce burden via cancer prevention? Asia-Pacific J Oncol Nurs 2022, 100066, https://doi.org/10.1016/j.apjon.2022.04.005 DOI: https://doi.org/10.1016/j.apjon.2022.04.005
Glanz K, Bishop DB. The Role of behavioral science theory in development and implementation of public health interventions. Annu Rev Public Health 2010;31:399–418. http://dx.doi.org/101146/annurev.publhealth012809103604 DOI: https://doi.org/10.1146/annurev.publhealth.012809.103604
Anwar Tayel A, Hosny H, Sherbini E, Abd A, Fattah E, Shosha A, et al. The effect of applying preventive intervention based on champion health believe model on breast cancer fatalism, knowledge and screening behaviors among female employees. Am J Nurs Res 2019;7(5):759–70. https://doi.org/10.12691/ajnr-7-5-9
Stacey FG, James EL, Chapman K, Courneya KS, Lubans DR. A systematic review and meta-analysis of social cognitive theory-based physical activity and/or nutrition behavior change interventions for cancer survivors. J Cancer Surviv 2015, 9:305–38. https://doi.org/10.1007/s11764-014-0413-z DOI: https://doi.org/10.1007/s11764-014-0413-z
Scruggs S, Mama SK, Carmack CL, Douglas T, Diamond P, Basen-Engquist K. Randomized trial of a lifestyle physical activity intervention for breast cancer survivors: effects on transtheoretical model variables. Health Promot Pract 2018;19(1):134–44.
https://doi.org/10.1177/1524839917709781 DOI: https://doi.org/10.1177/1524839917709781
Michie S, Atkins L, West R. The behaviour change wheel. A guide to designing interventions. 1st Ed. Silverback Publishing; 2016. 1003–1010 p.
Paalosalo-Harris K, Skirton H. Mixed method systematic review: The relationship between breast cancer risk perception and health-protective behavior in women with family history of breast cancer. Journal of Advanced Nursing 2017, 73: 760–74. https://doi.org/10.1111/jan.13158 DOI: https://doi.org/10.1111/jan.13158
Jones CL, Jensen JD, Scherr CL, Brown NR, Weaver CR, Weaver J. The health belief model as an explanatory framework in communication research: exploring parallel, serial, and moderated mediation. Health Communication 2015;30(6):2121–30.
https://doi.org/10.1080/10410236.2013.873363 DOI: https://doi.org/10.1080/10410236.2013.873363
Howlett N, Trivedi D, Troop NA, Chater AM. Are physical activity interventions for healthy inactive adults effective in promoting behavior change and maintenance, and which behavior change techniques are effective? A systematic review and meta-analysis. Transl Behav Med. 2019;9(1):147–57. https://doi.org/10.1093/tbm/iby010 DOI: https://doi.org/10.1093/tbm/iby010
Spector D. Lifestyle behaviors in women with a BRCA1 or BRCA2 genetic mutation: an exploratory study guided by concepts derived from the Health Belief Model. Cancer Nurs. 2007;30(1). https://doi.org/10.1097/00002820-200701000-00015 DOI: https://doi.org/10.1097/00002820-200701000-00015
Kinney AY, Gammon A, Coxworth J, Simonsen SE, Arce-Laretta M. Exploring attitudes, beliefs, and communication preferences of Latino community members regarding BRCA1/2 mutation testing and preventive strategies. Genet Med. 2010;12(2):105–15.
https://doi.org/10.1097/GIM.0b013e3181c9af2d DOI: https://doi.org/10.1097/GIM.0b013e3181c9af2d
Roberts AL, Crook L, George H, Osborne K. Two-month follow-up evaluation of a cancer awareness training workshop (“Talk Cancer”) on cancer awareness, beliefs and confidence of front-line public health staff and volunteers. Prev Med Reports. 2019;13:98–104.
https://doi.org/10.1016/j.pmedr.2018.11.017 DOI: https://doi.org/10.1016/j.pmedr.2018.11.017
Grimmett, C., Corbett, T., Brunet, J. et al. Systematic review and meta-analysis of maintenance of physical activity behaviour change in cancer survivors. Int J Behav Nutr Phys 2019, 16 (37):1-20. https://doi.org/10.1186/s12966-019-0787-4 DOI: https://doi.org/10.1186/s12966-019-0787-4
Hagger MS, Weed M. Debate: Do interventions based on behavioral theory work in the real world? Int J Behav Nutr Phys Act. 2019;16(1):1–10. https://doi.org/10.1186/s12966-019-0795-4 DOI: https://doi.org/10.1186/s12966-019-0795-4
Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot 1997;12(1):38–48. https://doi.org/10.4278/0890-1171-12.1.38 DOI: https://doi.org/10.4278/0890-1171-12.1.38
Descargas
Publicado
Cómo citar
Número
Sección
Licencia
Derechos de autor 2022 Diez De los Ríos de la Serna C, Fernández-Ortega P

Esta obra está bajo una licencia internacional Creative Commons Atribución-NoComercial-SinDerivadas 4.0.
Magna Scientia UCEVA proporciona un acceso abierto, libre y gratuito a su contenido, basado en el principio de que ofrecer al público un acceso libre a las investigaciones, ayuda a un mayor intercambio global del conocimiento. Lo cual, implica que los usuarios pueden leer, descargar, almacenar, imprimir, buscar, indexar y realizar enlaces a los textos completos de esta revista. Se permite distribuir los diversos artículos en las versiones post-print y oficial, sin previo permiso del autor o editor, considerando que el fin de este, no implica fines comerciales, ni la generación de obras derivadas; Solo se solicita la mención de la fuente así como la autoría. El titular del copyright será el o los autores que publiquen en Magna Scientia UCEVA.
Magna Scientia UCEVA está distribuida bajo los términos de la licencia https://creativecommons.org/licenses/by-nc-nd/4.0/deed.es