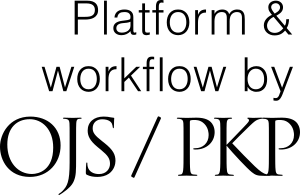
Choledochal cyst with prenatal diagnosis and postnatal management: A case report
DOI:
https://doi.org/10.54502/msuceva.v2n2a2Palabras clave:
Biliary atresia, Biliary cystic malformation, Choledochal cyst, Prenatal diagnosis, neonate, rare malformationsResumen
Cystic dilatation of the bile duct is part of a wide spectrum of biliary pathology with different etiopathogenic mechanisms. Choledochal cysts are rare malformations of the bile ducts. It is diagnosed in most cases during early childhood, although it can present at any age of life. The clinical presentation is variable and can be manifested by abdominal pain, palpable mass, cholestatic jaundice or by symptoms linked to the development of some of its complications: pancreatitis, cholangitis or rupture. The diagnosis is made through abdominal ultrasound and is completed with a ,magnetic cholangiography the recommended treatment is complete surgical resection that prevents the appearance of complications. A case of ultrasound prenatal diagnosis is presented at 29 weeks of gestation along with its evolution, management and postnatal treatment, it is also the first case in this health center located in Valle del Cauca
Descargas
Métricas
Citas
Baison GN, Bonds MM, Helton WS, Kozarek RA. Choledochal cysts: Similarities and differences between Asian and Western countries. World J Gastroenterol 2019;25:3334–43. https://doi.org/10.3748/wjg.v25.i26.3334
Huerta Sáenz I, Elías J, Torres E. Quiste de colédoco fetal: diagnóstico prenatal y manejo perinatal. Rev Per Ginecol Obstet 2013;59:59–62. DOI: https://doi.org/10.31403/rpgo.v59i22
http://www.scielo.org.pe/pdf/rgo/v59n1/a10v59n1.pdf.
Giha S, Redondo Y, Quintero G. Quiste de colédoco: diagnóstico y manejo intraoperatorio. Pediatria (Bucur) 2016;49:64–7.
https://doi.org/10.1016/j.rcpe.2016.04.004 DOI: https://doi.org/10.1016/j.rcpe.2016.04.004
Corrochano M, LLanos R, García A. Quiste de colédoco en una lactante de tres meses de edad: diagnóstico prenatal y manejo quirúrgico. Rev Pediatr Esp 2013;4:84–8. https://wp-intercienciamedica-prd.azurewebsites.net/wp-content/uploads/2021/07/Quiste-de-coledoco-en-una-lactante-de-tres-meses-de-edad-diagnostico-prenatal-y-manejo-quirurgico.pdf.
Soares KC, Arnaoutakis DJ, Kamel I, Rastegar N, Anders R, Maithel S, et al. Choledochal Cysts: Presentation, Clinical Differentiation, and Management. J Am Coll Surg 2014;219:1167–80. https://doi.org/10.1016/j.jamcollsurg.2014.04.023 DOI: https://doi.org/10.1016/j.jamcollsurg.2014.04.023
López Ruiz R, Aguilera Alonso D, Muñoz Aguilar G, Fonseca Martín R. Quistes de colédoco, una causa inusual de ictericia en pediatría. Presentación de serie de casos. Rev Chil Pediatr 2016;87:137–42.
https://doi.org/10.1016/j.rchipe.2015.08.009 DOI: https://doi.org/10.1016/j.rchipe.2015.08.009
Peñaloza- Ramírez A, Coral- Argoty E, Castro- Rodríguez M, Álvarez- Gil J, Aponte-Ordoñez P. Disfunción del esfínter de Oddi: un reporte de caso. Rev Colomb Gastroenterol 2021;36:52–8. https://doi.org/10.22516/25007440.550 DOI: https://doi.org/10.22516/25007440.550
Sugita R. Pancreaticobiliary reflux as a high-risk factor for biliary malignancy: Clinical features and diagnostic advancements. World J Hepatol 2015;7:1735. https://doi.org/10.4254/wjh.v7.i13.1735 DOI: https://doi.org/10.4254/wjh.v7.i13.1735
Calzadilla J, Sanhueza N, Farías S, González F. Recurrent pancreatitis secondary to sphincter of Oddi dysfunction: case report. Medwave 2016;16:e6585–e6585. https://doi.org/10.5867/medwave.2016.09.6585 DOI: https://doi.org/10.5867/medwave.2016.09.6585
Machado K, Cascino C, Ghione A, Montano A. Quiste de colédoco. Presentación en un lactante con fiebre. Caso clínico. Arch Pediatr Urug 2011;82:23–8. http://www.scielo.edu.uy/pdf/adp/v82n1/v82n1a05.pdf
Singham J, Yoshida EM, Scudamore CH. Choledochal cysts: part 1 of 3: classification and pathogenesis. Can J Surg 2009;52:434–40. PMID:19865581.
DeJesus J, Hughes B, Geisler E, Defilippo C, Gaffey J, Radhakrishnan RS. Type II choledochal cyst of the cystic duct in a 3-month-old. J Pediatr Surg Case Rep 2022;86:102440. https://doi.org/10.1016/j.epsc.2022.102440 DOI: https://doi.org/10.1016/j.epsc.2022.102440
Farías Molina SM, Castillo Machado RL, Sanhueza Palma NC, Calzadilla Riveras JA. Todani choledochal cyst type II: case report and review. Medwave 2016;16:e6583–e6583. https://doi.org/10.5867/medwave.2016.09.6583 DOI: https://doi.org/10.5867/medwave.2016.09.6583
Torres M, Becerra M, Calderón B, Salinas I, Ruiz M, Ventura J. Choledochal Cyst. Biliary Tract - Review and Recent Progress [Working Title], IntechOpen; 2022. https://doi.org/10.5772/intechopen.106451 DOI: https://doi.org/10.5772/intechopen.106451
Baison GN, Bonds MM, Helton WS, Kozarek RA. Choledochal cysts: Similarities and differences between Asian and Western countries. World J Gastroenterol 2019;25:3334–43. https://doi.org/10.3748/wjg.v25.i26.3334 DOI: https://doi.org/10.3748/wjg.v25.i26.3334
Dezerega P, Sepúlveda E, González G, Pérez P, Jara M, Vásquez M. Tumores fetales: II parte. Rev Chilena Ultras 2006;9:24–33.
http://www.sochumb.cl/wp-content/uploads/2018/06/US-10-2-2007-b.pdf.
Gürsoy Çoruh A, Gülpınar B, Baş H, Erden A. Frequency of bile duct confluence variations in subjects with pancreas divisum: an analysis of MRCP findings. Diagn Interv Radiol 2018;24:72–6. https://doi.org/10.5152/dir.2018.17200 DOI: https://doi.org/10.5152/dir.2018.17200
Kim JY, Kim HJ, Han HY. A Case Report of an Unusual Type of Choledochal Cyst with Choledocholithiasis: Saccular Dilatation of the Confluent Portion of Both Intrahepatic Ducts. Journal of the Korean Society of Radiology 2015;73:252.
https://doi.org/10.3348/jksr.2015.73.4.252 DOI: https://doi.org/10.3348/jksr.2015.73.4.252
Kumar M, Rajagopalan S. Choledochal cyst. Med J Armed Forces India 2012;68:296–8.
https://doi.org/10.1016/j.mjafi.2012.04.011 DOI: https://doi.org/10.1016/j.mjafi.2012.04.011
Hamid R, Bhat NA, Ahmad M, Singh B. Choledochal Cyst (CDC). Gastrointestinal Surgery - New Technical Proposals, InTech; 2018.
https://doi.org/10.5772/intechopen.72938 DOI: https://doi.org/10.5772/intechopen.72938
Whitworth M, Bricker L, Mullan C. Ultrasound for fetal assessment in early pregnancy. Cochrane Database Syst Rev 2015;2015:CD007058.
https://doi.org/10.1002/14651858.CD007058.pub3 DOI: https://doi.org/10.1002/14651858.CD007058.pub3
Carlson LM, Vora NL. Prenatal Diagnosis: Screening and Diagnostic Tools. Obstet Gynecol Clin North Am 2017;44:245–56.
https://doi.org/10.1016/j.ogc.2017.02.004 DOI: https://doi.org/10.1016/j.ogc.2017.02.004
Bricker L, Medley N, Pratt JJ. Routine ultrasound in late pregnancy (after 24 weeks’ gestation). Cochrane Database Syst Rev 2015;2015:CD001451. https://doi.org/10.1002/14651858.CD001451.pub4 DOI: https://doi.org/10.1002/14651858.CD001451.pub4
Wilson ECF, Wastlund D, Moraitis AA, Smith GCS. Late pregnancy ultrasound to screen for and manage potential birth complications in nulliparous women: a cost-effectiveness and value of information analysis. Value in Health 2021;24:513–21. https://doi.org/10.1016/j.jval.2020.11.005 DOI: https://doi.org/10.1016/j.jval.2020.11.005
Descargas
Publicado
Cómo citar
Número
Sección
Licencia
Derechos de autor 2022 Medina Torres and Hincapié Álvarez

Esta obra está bajo una licencia internacional Creative Commons Atribución-NoComercial-SinDerivadas 4.0.
Magna Scientia UCEVA proporciona un acceso abierto, libre y gratuito a su contenido, basado en el principio de que ofrecer al público un acceso libre a las investigaciones, ayuda a un mayor intercambio global del conocimiento. Lo cual, implica que los usuarios pueden leer, descargar, almacenar, imprimir, buscar, indexar y realizar enlaces a los textos completos de esta revista. Se permite distribuir los diversos artículos en las versiones post-print y oficial, sin previo permiso del autor o editor, considerando que el fin de este, no implica fines comerciales, ni la generación de obras derivadas; Solo se solicita la mención de la fuente así como la autoría. El titular del copyright será el o los autores que publiquen en Magna Scientia UCEVA.
Magna Scientia UCEVA está distribuida bajo los términos de la licencia https://creativecommons.org/licenses/by-nc-nd/4.0/deed.es